American Society of Clinical Oncology (ASCO 2021)
The American Society of Clinical Oncology (ASCO) annual meeting is the world’s largest and most renowned cancer conference. In years past, it has brought together the worlds most respected and innovative cancer researchers, including those from Breast Cancer Trials, under one roof to discuss the latest advancements in treatments, clinical trials research and cancer care.
However, due to the ongoing COVID-19 pandemic worldwide, the conference went virtual for its second year, allowing delegates to log in all over the world, at all hours of the day and night.
We have provided a summary of the key breast cancer clinical trials research presented, including the exciting Breast Cancer Trials OlympiA study results.
OlympiA Trial Results: New Treatment Reduces Breast Cancer Recurrence By 42% In Patients With Early-Stage Breast Cancer With An Inherited BRCA1 or BRCA2 Gene Abnormality
Results from the OlympiA clinical trial show that olaparib reduces breast cancer recurrence by 42% in patients with early-stage breast cancer who have a BRCA1 or BRCA2 gene mutation.
The OlympiA clinical trial was coordinated internationally by the Breast International Group and recruited 1,836 patients worldwide, including 60 women from Australia.
OlympiA found that giving olaparib tablets twice daily for a year to patients with BRCA1 and BRCA2 mutations, after they have completed chemotherapy, increases the chances that they will remain free of invasive or metastatic cancer. This was a phase III clinical trial, which tested the efficacy and safety of olaparib tablets versus placebo as adjuvant treatment for early-stage breast cancer at high risk of recurrence.
Participants could have either hormone receptor positive or negative cancer but had to be HER2 negative. The tablet was well tolerated, with manageable side effects including anaemia, low white blood cell count and mild nausea.
Professor Kelly-Anne Phillips is the Breast Cancer Trials Study Chair of the OlympiA clinical trial and says the results provide a new treatment option for patients with early-stage breast cancer.
“One of the biggest fears that patients have is that their breast cancer will come back. The OlympiA clinical trial has identified a new treatment for patients with early-stage breast cancer that have a genetic mutation in the BRCA1 or BRCA2 genes, which may help prevent their breast cancer returning and cancer spreading, after their initial treatment has been completed,” said Professor Phillips.
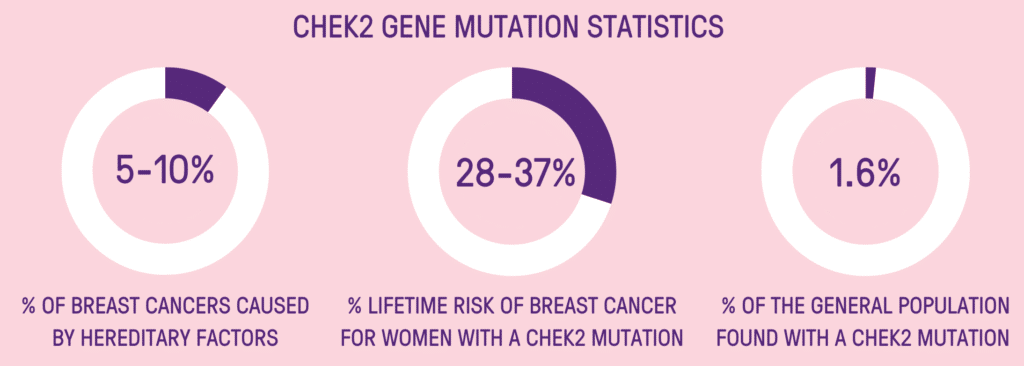
“Approximately 5% of all breast cancer patients have a BRCA1 or BRCA2 gene mutation, which equates to roughly 1,000 women diagnosed with breast cancer in Australia each year. These women are typically diagnosed with breast cancer at a younger age and often have a particularly aggressive form of breast cancer.
“Our study findings are a significant step forward in the precision treatment of breast cancer and provides a new treatment option.”
“The findings also mean that genetic testing for BRCA1 and BRCA2 will likely become more routine for all women with newly diagnosed breast cancer. This will have the downstream effect of helping us to identify their relatives who also have the gene abnormality and who can therefore undertake evidence-based treatments that can prevent them getting cancer. So this is not only a step forward in breast cancer treatment, but also in helping us to prevent cancer.”
CDK4/6 Inhibitors Boost Overall Survival In HR-Positive, HER2 Negative Advanced Breast Cancer
Updated results from two clinical trials PALOMA-3 and MONALEESA-3, support the use of fulvestrant plus a CDK4/6 inhibitor as standard of care for patients with HR positive, HER2 negative advanced breast cancer. Long-term follow-up of these studies showed this treatment combination could prolong the overall survival of patients with this type of advanced breast cancer.
In the PALOMA-3 study, 521 women with HR-positive, HER2 negative advanced breast cancer were randomised 2:1 to receive palbociclib (a CDK4/6 inhibitor) plus fulvestrant or fulvestrant plus placebo. Patients enrolled on the study had breast cancer that had progressed on or after endocrine therapy and had up to one prior chemotherapy treatment. In a follow-up taken at 73.3 months, the median overall survival was 34.8 months for those on the palbociclib arm compared with 28 months for those on the placebo. Five-year overall survival was 23.3% for those on palbociclib compared with 16.8% for those on the placebo.
Updated results from the MONALEESA-3 study showed that the median overall survival was 53.7 months for those on the ribociclib (CDK4/6 inhibitor) arm, compared with 41.5 months for those on the placebo. The five-year overall survival was 46% for the ribociclib arm compared with 31.1% for the placebo arm. This study enrolled 726 postmenopausal patient with HR-positive, HER2-negative patients. Patients were randomly assigned 2:1 to receive ribociclib plus fulvestrant or fulvestrant plus placebo. Because these two studies enrolled patients at different time-points in their treatment, with slightly different characteristics, the results cannot be compared to each other directly.
According to the researchers who worked on the studies, these combined results show that CDK4/6 inhibitors could help to prolong the overall survival of patients with advanced breast cancer.
De-Escalating Treatment For HR Negative HER2 Positive Breast Cancer
The overall survival analysis of the WSG-ADAPT HR-/HER+ study, has shown that treatment with targeted therapies pertuzumab (Perjeta) and trastuzumab (Herceptin), can be just as effective without adding 12 weeks of paclitaxel (a chemotherapy drug).
This clinical trial aimed to find out how to reduce the intensity of neoadjuvant (pre-surgical) treatment, safely and effectively, in patients with HR negative, HER2 positive early-stage breast cancer. A five-year follow-up showed that overall survival with chemotherapy was 98% and 94% without chemotherapy. Invasive disease-free survival was 98% on the added chemotherapy arm, compared with 87% without. None of these outcomes were statistically different. Further analyses showed that patients whose tumour was eradicated prior to breast surgery had excellent outcomes, irrespective of whether they received chemotherapy or not.
The researchers involved in this study looked to the tumour biomarkers to see if they could determine which patients could benefit from this de-escalated treatment. They concluded that future investigations of chemotherapy-free treatment regimens may need to be focused on select patients with sensitive tumors, such as those with HER2-positive, non-basal like tumours, early responders, and those with predictive RNA (gene) signatures. Trials such as ADAPT, COMPASS and a future Breast Cancer Trials clinical trial DECRESCENDO will continue to explore similar de-escalation strategies in patients with breast cancer.
Nearly Three-Quarters Of Breast Cancer Patients Are Undertaking Complementary Medical Treatments
A survey report, released in conjunction with ASCO 2021, has found that nearly three-quarters of breast cancer patients (73%) report using at least one type of complementary therapy after their cancer diagnosis. Meanwhile, less than half of oncologists (43%) believe their patients are engaging in this practice.
The survey polled 115 oncologists and 164 breast cancer patients. It found that 66% of oncologists and 65% of patients believe using complementary therapies improved patients’ quality of life. However, there was a difference in the type of therapies each group saw as useful. The oncologists believe nutrition consultation, support groups, psycho-oncology support and exercise consultation were the most important complementary health services. However, the medical professionals gave low marks to spiritual services and meditation or mindfulness, two approaches patients considered important.
Other Breast Cancer Trials Research Presented At ASCO
- PENELOPE-B did not show a benefit from the addition of one-year palbociclib to endocrine therapy compared to the placebo in the patient population of the trial – HR+, HER2 negative early breast cancer.
- APHINITY found that dual HER2 blockade with pertuzumab plus trastuzumab does not increase the risk of cardiac events compared with a placebo and trastuzumab alone.
- ALTTO found that in HER2+ early breast cancer patients enrolled on the trial, the PREDICT+ score greatly underestimated overall survival. The low performance of this prognosis tool was consistent across all patient subgroups, and therefore PREDICT+ should be used with caution to give prognostic estimation in HER2+ early breast cancer patients treated with effective chemotherapy and anti-HER2 targeted therapies.
QUICK ACCESS
American Society of Clinical Oncology 2021
CDK4/6 Inhibitors Boost Overall Survival In HR-Positive, HER2 Negative Advanced Breast Cancer
De-Escalating Treatment For HR Negative HER2 Positive Breast Cancer
Nearly Three-Quarters Of Breast Cancer Patients Are Undertaking Complementary Medical Treatments
Support Us
Help us to change lives through breast cancer clinical trials research