Breast lymphoedema is the build-up of lymphatic fluid in the breast and/or chest wall. This can lead to swelling, discomfort, and changes in skin texture. This can develop when the lymphatic system is damaged or disrupted, by breast cancer itself or following breast cancer treatments such as surgery, lymph node removal, or radiation therapy that may damage or disrupt the lymphatic system. This condition is distinct from the more widely known arm lymphoedema and may occur even when arm swelling is not present.
For many, breast lymphoedema develops gradually, sometimes appearing weeks, months or even years after treatment. Lymphoedema of the breast is usually caused by treatment rather than the cancer itself. While it may not be life-threatening, it can significantly affect quality of life if not managed. People who have experienced lymphoedema after breast cancer surgery should be aware of the signs and seek early advice from their healthcare team.
At Breast Cancer Trials, we are dedicated to improving treatment outcomes and managing side effects particularly through treatment optimisation.
What Does Breast Lymphoedema Look Like?
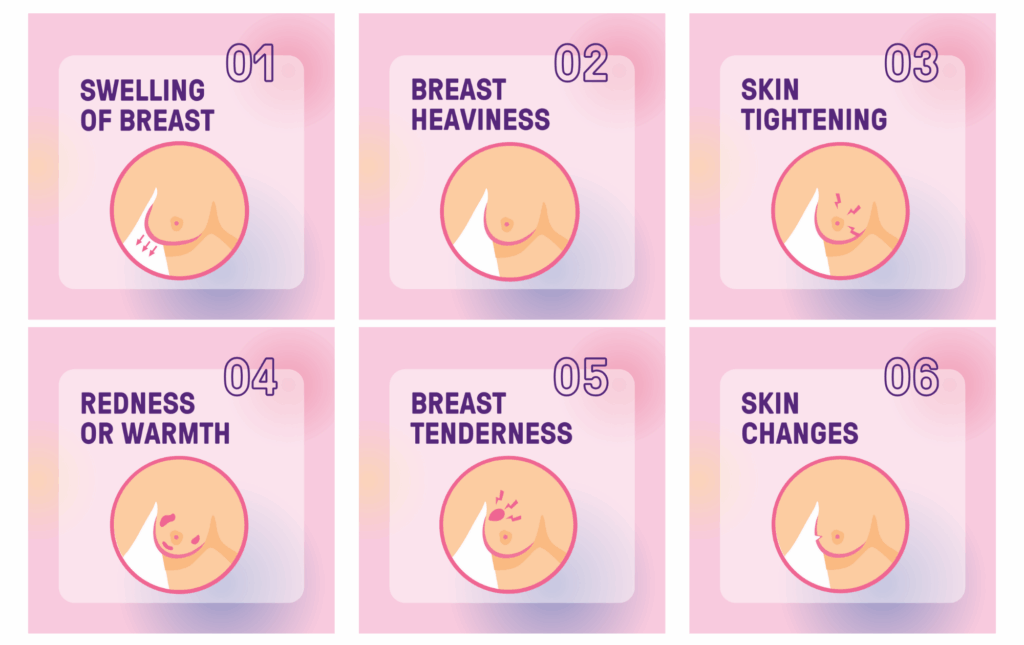
The appearance and feel of breast lymphoedema can vary. Common breast lymphoedema symptoms include:
- Swelling or puffiness in the breast
- Feelings of heaviness or fullness
- Tightness in the skin or surrounding breast tissue
- Redness or warmth
- Tenderness when touched
Less common breast lymphoedema symptoms include:
- Skin thickening
- Dimpling
- Or changes in texture over time
These symptoms can be subtle and may fluctuate, so familiarity with what is normal for you is important for early detection.
While this guide is designed to help you recognise the signs, it is important to remember that symptoms can be confused with other conditions, such as infection, inflammation, breast cancer recurrence, or the skin effects of radiation treatment. Knowing what breast lymphoedema looks like and the symptoms can help individuals and healthcare providers distinguish it from these other concerns and seek appropriate treatment sooner. Early detection can improve comfort and reduce the risk of lymphoedema progression, reaffirming the importance of seeking medical advice promptly.
How Common is Breast Lymphoedema?
Breast lymphoedema occurs less frequently than arm lymphoedema. It is more likely after treatments that affect lymphatic drainage, including axillary surgery, radiation therapy to the chest wall, and infections or injuries in the breast area after treatment.
Australian studies and clinical experience indicate the condition is often underdiagnosed, partly because symptoms may be mild or delayed. While Breast Cancer Trials does not conduct research specifically into breast lymphoedema incidence, many of our clinical trials focus on treatment optimisation to improve quality of life and reduce treatment side effects wherever possible.
What Percentage of Breast Cancer Patients Get Lymphoedema?
An Australian survey conducted via Breast Cancer Network Australia found that 35% of women reported having lymphoedema after breast cancer treatment, with an additional 9% unsure whether they had it. This highlights the likelihood of underdiagnosis and the need for improved awareness.
In addition, Cancer Council Australia notes that one study estimated lymphoedema occurs in about 20% of people treated for cancers such as breast, melanoma, gynaecological, or prostate cancers. While this percentage includes lymphoedema in areas other than the breast, it reinforces that lymphoedema is a common side effect of cancer treatment.
Breast lymphoedema is a side effect for people treated for breast cancer, regardless of whether they have a mastectomy or breast-conserving surgery (also known as a lumpectomy). Because the risk is present across treatment types, it’s important for anyone who has undergone surgery and/or radiation to be aware of early signs and to have regular follow-up, so that any lymphoedema can be managed promptly.
Causes of Breast Lymphoedema
Breast lymphoedema develops when lymphatic drainage is disrupted, leading to fluid build-up in breast tissue. This may occur after lymph node removal (sentinel node biopsy or axillary clearance) and radiation therapy, and can be worsened by trauma to lymphatic vessels, inflammation, scar tissue, or fibrosis.
Certain chemotherapy drugs, infections, or injury to the breast or chest area post-treatment can also contribute. A related condition, known as cording after breast cancer, can sometimes occur alongside or after breast lymphoedema.
Breast Lymphoedema After Radiation
Radiation can damage lymphatic vessels, narrowing or scarring them and reducing fluid drainage. People who receive radiation to the breast, chest wall, axilla, or collarbone area may develop breast lymphoedema months or even years after treatment.
The EXPERT clinical trial, led by Breast Cancer Trials, is investigating whether some people can safely avoid radiotherapy after breast cancer surgery. By identifying those who may not need radiation, the trial aims to help them avoid potential side effects, including breast lymphoedema.
How to Avoid Lymphoedema After Lymph Node Removal
Although there is no guaranteed way to avoid breast lymphoedema, adopting certain strategies can reduce your risk. Recommendations for the prevention of breast lymphoedema include:
- Maintaining good skin health to prevent infection
- Avoiding injuries or burns to the breast or chest area
- Wearing supportive and well-fitting bras
- Keeping physically active
- Maintaining a healthy weight
For people looking at how to avoid lymphoedema after lymph node removal, gentle stretching and strengthening exercises approved by a physiotherapist can help keep lymph fluid moving. Early reporting of swelling or changes to your doctor remains the most important step.
Breast Lymphoedema Compression and Other Management Options
Breast lymphoedema compression therapy is one of the most effective ways to manage swelling and improve comfort. Compression garments for lymphoedema, such as specially designed bras or pads, apply gentle pressure to the affected area to help move lymph fluid away from the breast.
For people with both breast and arm swelling, compression arm sleeves for lymphoedema are available through hospitals, lymphoedema clinics, and medical suppliers. Management may also include:
- Manual lymph drainage by a qualified therapist
- Gentle exercise
- Skin care routines to prevent infection
- Temporary bandaging
Frequently Asked Questions
What’s the difference between primary and secondary lymphoedema?
Primary lymphoedema is caused by a genetic condition affecting the lymphatic system. Secondary lymphoedema develops after damage to the lymphatic system, such as from breast cancer treatments. Breast lymphoedema is considered to be a secondary lymphoedema.
Do compression sleeves help with breast lymphoedema?
Compression sleeves may help if swelling extends to the arm. For breast-only lymphoedema, a compression bra or pad is often more suitable to provide compression to the affected area and encourage drainage away from this area.
Is lymphoedema cancer?
No – lymphoedema is not cancer. It is a condition caused by a build-up of lymphatic fluid in tissues due to problems with the lymphatic system.
Can lymphoedema be cured?
While breast lymphoedema can’t always be permanently cured, symptoms can often be well managed. With breast lymphoedema treatment and self-care, swelling can reduce and comfort can improve.
Sources:
https://www.racgp.org.au/getattachment/5a01a899-35fd-47fe-a1c8-806be1967121/Breast-cancer-related-lymphoedema.aspx
https://www.cancer.org.au/assets/pdf/understanding-lymphoedema
Breast Cancer Trials and Ongoing Research
At Breast Cancer Trials, we are committed to clinical research that optimises treatments to improve quality of life and reduce side effects, so that no lives are cut short by breast cancer.
Several of our current studies are focused on treatment optimisation, including trials like EXPERT, which is investigating whether some patients can safely avoid radiotherapy; PROSPECTIVE, which aims to find out if surgery without radiotherapy will still be effective at stopping the cancer coming back and reduce the side effects and cost of usual treatment; and OPTIMA, which is exploring how to tailor chemotherapy use more precisely. These studies aim to improve outcomes while reducing the impact of treatment side effects.
If you’d like to learn more about our current research or how to get involved, you can explore details about these trials and other opportunities to participate, or sign up for our researcher’s newsletter via the form below to stay up to date.