The Impact Of A Diagnosis
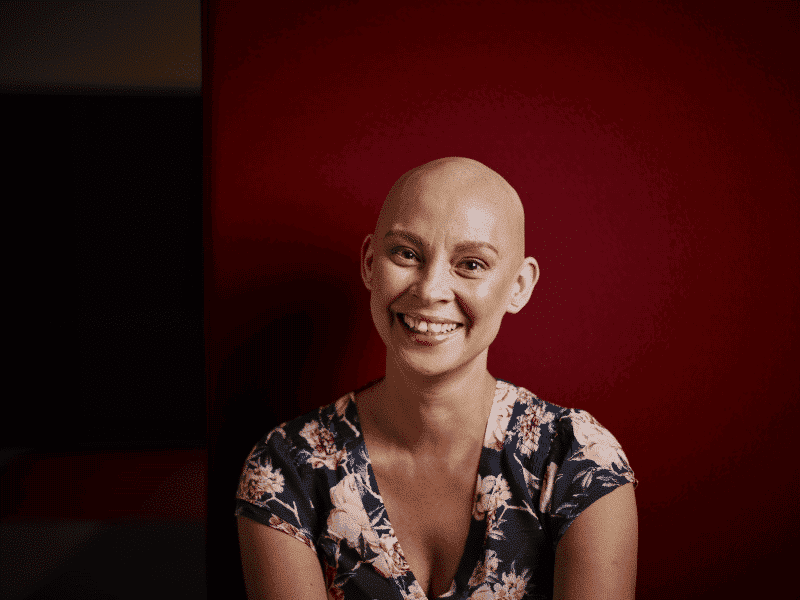
A breast cancer diagnosis is an incredibly traumatic event in a person’s life.
The psychological impact of a diagnosis can be significant if a patient’s mental health is not looked after.
However, there is no one-size fits all approach to mental health in this area as everyone will react to their diagnosis differently according to Dr Lisa Beatty, a clinical psychologist and Cancer Council South Australia Senior Research Fellow.
“We do know that the distress rates are roughly 4 in 10 women will have what we call clinically significant distress and that is where it is actually getting to the point where it might be causing a real impact in how they’re able to function in their life.”
“It might be that it’s stopping them from going out and socialising, it might be that it’s stopping them from working and this is on top of the impact of the cancer itself.”
“We also know there can be huge issues with body image, we know that there are big issues with feeling shock and anger. And also one of the big things we’re hearing a lot more now is that women might not necessarily feel like they’re being particularly well supported, that some of the people that they thought would be their core support people would just disappear and other people that they hadn’t necessarily expected to be involved, really put their hands up.”
“The number of times I hear people say that a breast cancer diagnosis really shows them who their true friends are… It’s a very common finding.”
Unfortunately demand for mental health services far outweighs the supply in the cancer space.
Dr Beatty said access to cancer specific mental health services can be very dependent on the institution or hospital you are receiving treatment at.
“Some of the big metro-based hospitals with big cancer services will have a lot of funding for psycho-oncology, so you might have a team of people there that you can be referred to.”
“The hospital where I work, I am the only psychologist that works in cancer and I’m funded to do one day per week.”
“So, as you can imagine, it can mean that there are really long wait lists.”
“The demand is very much exceeding the available supply.”
Dr Beatty said because of this, it is not always routine for patients to be referred to these services.
“I think in some hospitals where there isn’t any (services), it leaves a bit of an ethical dilemma for some of the clinicians.”
“Do they screen for distress when they don’t have anywhere to send people afterwards?” she said.
“So, we try and work in a very integrated fashion as part of the multi-disciplinary team.”
Listen to the podcast
Clinical psychologist Dr Lisa Beatty explains what impact a diagnosis can have, how to can get help & what impact poor mental health can have on your recovery.
How Poor Mental Health Can Affect Cancer Treatment And Recovery
Dr Beatty said psychology is increasingly being seen as a core component to a patient’s overall health.
“We know that it impacts deeply not only on people’s well-being but can actually impact on medical outcomes as well, that there is an increased severity and prevalence of physical symptoms and side effects, increased severity of toxicity, when people are feeling depression, anxious or distressed.”
“So, it is being increasingly recognised that we need to actually screen and address distress.”
“It’s not an optional extra.”
“It’s a core component.”
Dr Beatty said there can be a significant impact upon a patient’s response to treatment if their mental health is not considered during their diagnosis and treatment.
“We do know there is a three-fold reduction in adherence to their anti-cancer treatment for people who have untreated distress and that can also lead to some of the recent meta-analysis which has shown there is a 17% increase in mortality rates when people have untreated depression.”
How To Get Mental Health Help When You’ve Been Diagnosed With Breast Cancer
Dr Beatty said if the hospital or institution you are being treated at has a psychologist, you can be referred there directly.
“So, if there is a psychologist associated with the hospital, there won’t be any out-of-pocket costs for it.”
“They will actually just get a referral through their oncologist directly to that psychologist.”
However, if there is no psychologist at your treating hospital, you are still able to get help.
Dr Beatty said they are working to upskill community-based psychologists to treat cancer related mental health issues.
“One of the challenges and something we’re trying to work on here in Australia, is actually up-skilling the community based psychologists in how-to-treat depression and anxiety in cancer, so that we can actually make use of that Medicare funded system, the Better Access system, and get people treated by some of these community based psychologists as well.”
“However, there can then be out-of-pocket costs in this system.”
Dr Beatty said there are many things an individual can do to help ease their own burden.
“I think first of all, it’s really normal to struggle.”
“So, I’ve been talking about the 30 to 40 per cent of people that get clinically significant distress, I would say it’s more upwards of 90 to 100% that would struggle when they’re first diagnosed.”
“So, recognise that it is perfectly normal, it doesn’t make it enjoyable while you’re stuck in it.
But, it will, over time, reduce in severity.”
She also said its important to speak up and ask for help if you can.
“Make sure you are an advocate and speak up, if you feel comfortable doing so, to your treatment team.”
“There are a lot of other allied health options.”
“Also, some of the basic things you can do to really look after yourself, both your physical and your mental health is exercise,” she said.
“Don’t underestimate the role of that, that’s a very affordable and effective treatment for both your mental and physical health after your diagnosis.”
Support Us
Help us to change lives through breast cancer clinical trials research