Dr Holly Keane is a Breast Surgeon at the Peter MacCallum Cancer Centre in Melbourne, with an interest in the areas of pain management and tailored screening for breast cancer patients.
We spoke with Dr Keane about pain after breast cancer therapy, its implications in day-to-day life for breast cancer patients, and some ways to reduce pain during recovery.
“Pain, including post mastectomy pain syndrome, is something that I’ve looked into quite substantially. I’m also very interested in the screening of high-risk women and tailored screening. All of these projects I started working on within my fellowship in San Francisco and I’m trying to continue back in Melbourne, Australia.”
How common is pain after breast cancer therapy? Is it something that affects everyone?
“So, I wouldn’t say all women, but it is a majority. In the literature, the incidence of post mastectomy pain syndrome is between 25% to 60%, but I think it could be even higher than that simply because clinicians don’t always ask about it and it’s not always identified or documented.”
What are some ways that people can reduce pain after breast cancer therapy?
“So, the lifestyle interventions that we talk about include exercise and having a normal weight, but that isn’t specific to post mastectomy pain. It’s not really been shown to decrease that incidence, but it improves breast cancer specific survival, and we know that it improves outcomes during chemotherapy and other breast cancer treatments.”
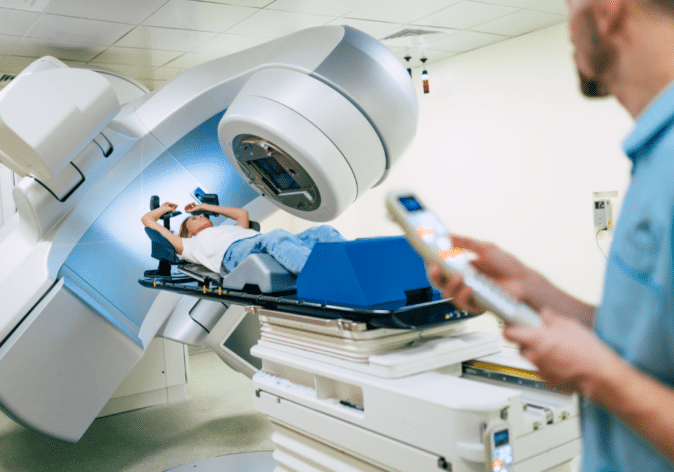
“But the ways to specifically reduce pain can include oral painkillers, some neuropathic pain tablets work as well. But my interest and what I was talking about at the Breast Cancer Trials conference this year was an injection specifically into the nerve that is cut during mastectomy, that comes out of the chest wall and it forms a little neuroma, which can be targeted with local anesthetic and with the steroid injection to decrease this neuropathic pain.”
“So, simply we must get clinicians, surgeons, oncologists, radiation oncologists just to ask about the presence of these symptoms. Asking the patient what type of pain they’re experiencing, is the pain felt under light touch or are they experiencing constant pain over the mastectomy field or over the breast or reconstructed breast.”
“Once you know the answer, if the patient said yes, that they do get that sort of pain, you just simply examine the patient in the clinic room. So, they just lie down, you palpate along the inframammary fold. And if there’s what’s called a ‘trigger point’, which is when you palpate with your index finger and your thumb and the patient sort of hits the roof with pain, you know that there’s a neuroma lying underneath. From there you can simply grab a syringe with the local anesthetic and the steroid in the mix in the syringe and inject it directly into the patient. And many women will have instant results, which is very important and extremely impactful for them.”
“So, we should ask about it with everyone who’s had breast cancer surgery. Hopefully we can get the word out that this is available and is opportunity for all patients. People who treat breast cancer need to be aware of this intervention, and everyone should be able to do it including surgeons and you know other physicians as well.”
“People’s faces, you know, and their instant reactions tell us that it is life changing. As I mentioned in the talk yesterday, things like seatbelts or even clothes and bras can irritate and accentuate this pain, and it can be changed with this simple intervention.”
Listen to the Podcast
We spoke with Dr Holly Keane about pain after breast cancer therapy, its implications in day-to-day life for breast cancer patients, and some ways to reduce pain during recovery.
As an addition to this, how important is diet and exercise in reducing pain after breast cancer therapy?
“So, there isn’t great evidence specifically for post-mastectomy pain, but certainly to help women get through chemotherapy, endocrine therapy, and radiotherapy, exercise and diet is helpful and certainly exercise increases resistance to specific pain.”
“So, I would encourage all my patients to regularly exercise and it’s going to be moderate to high intensity exercise, three to four times a week. So, getting your heart rate up and sweating. In terms of diet, I mean we heard about diet yesterday during one of the talks. There are some links, but certainly a well-balanced diet is strongly encouraged.”
What advice would you give to a patient who was experiencing this sort of pain after their breast cancer therapy?
“Most importantly, let your specialist know, and then hopefully they will be aware of this simple intervention, and if they aren’t able to provide the intervention themselves, they can refer you to a surgical oncologist to be able to perform the injection.”
What are your hopes for the future of breast cancer research?
“That’s a good broad question. Really, my hope is in the prevention setting. You know, we do focus on this area quite a lot and have to because breast cancer is so common. There is a large focus on the treatment of early breast cancer, then the adjuvant treatments, and then unfortunately, if it gets to the metastatic stage, we need to consider all the different drug combinations and changes.”
“But we really need to be preventing this before it happens, so we don’t have to do all these highly scientific drug trials. If we can prevent more cancers from occurring, this will have a great outcome and that is why I think we should really focus a lot of our research on prevention, because we won’t need all these extra treatments if we can prevent it in the beginning.”
Support Us
Help us to change lives through breast cancer clinical trials research