The Importance of Breast Cancer Screening
The earlier breast cancer is found, the better the chance of survival. Screening mammography can detect breast cancer at its earliest state, before it can be felt.
BreastScreen Australia recommends women aged 50-74 without breast cancer symptoms should have a screening mammograms every two years. This is the targeted age group as more than 75% of breast cancers occur in women aged over 50. Women aged 40-49 and 75 and over are eligible to receive free mammograms but do not receive an invitation to attend.
In New Zealand, women aged between 45 and 69 years are able to receive a free mammogram every two years.
Ways to Prevent Breast Cancer
Medical Interventions
There are several medical interventions available to help prevent breast cancer, particularly for individuals at higher risk due to genetic factors, family history, or other risk factors. These interventions include medications, surgeries, and other medical strategies based on an individual’s risk profile.
- Risk-reducing medications: Certain medications can help lower the risk of developing breast cancer, especially those that are hormone-receptor positive. These can include tamoxifen, anastrozole, and exemestane.
Surgical Options
For individuals with a very high risk (e.g., BRCA1/BRCA2 mutation carriers), surgery can dramatically reduce the risk of breast cancer.
- Prophylactic (Preventive) Mastectomy: Involves the surgical removal of one or both breasts before cancer develops. Reduces breast cancer risk by up to 95% in high-risk individuals.
Removing Ovaries to Prevent Breast Cancer
A Prophylactic Oophorectomy is the removal of the ovaries and fallopian tubes to lower estrogen levels, reducing the risk of both breast and ovarian cancers. This is often recommended for women with genetic mutations like BRCA1/2, especially after childbearing.
Benefits of Oopherectomy:
- Reduced Cancer Risk: For premenopausal women, oophorectomy lowers estrogen levels, reducing the risk of hormone-receptor-positive breast cancer by up to 50%. In relation to ovarian cancer, reduces the risk by up to 95% in high-risk individuals (e.g., BRCA mutation carriers).
- Improved Survival: Studies suggest that prophylactic oophorectomy can significantly increase life expectancy for women with genetic predispositions to breast or ovarian cancer.
- Simplicity of Proceedure: An oopherectomy is a relatively straightforward surgical procedure, often performed laparoscopically (minimally invasive), with a shorter recovery time than more extensive surgeries.
- Eliminated Future Ovarian Issues: Prevents benign (non-cancerous) ovarian conditions, such as ovarian cysts or endometriosis, which can require further treatment.
Risk Associated with Oopherectomy:
- Surgical Risks: This can include typical risks of surgery such as bleeding, infection, and adverse reactions to anesthesia. Rare complications associated with surgical proceedures can include damage to nearby organs like the bladder or intestines.
- Premature Menopause: Unfortinately for premenopausal women, oophorectomy causes immediate menopause. Symptoms include hot flashes, night sweats, vaginal dryness, mood swings, and sleep disturbances. This may increase the risk of osteoporosis, heart disease, and cognitive decline due to the loss of estrogen.
- Impact on Fertility: Permanently ends the ability to conceive naturally, which can be a significant consideration for younger women.
- Potential Psychological Impacts: Loss of fertility and the sudden onset of menopause can lead to feelings of grief, anxiety, or depression. Some women may experience a reduced sense of femininity or sexual confidence.
- Residual Cancer Risk: Oophorectomy does not eliminate all cancer risk. There’s still a slight chance of developing primary peritoneal cancer (a rare cancer that arises in the lining of the abdomen, which shares origins with ovarian tissue).
Removing Breast Tissue to Prevent Breast Cancer
A prophylactic mastectomy is the surgical removal of one or both breasts in individuals who do not have breast cancer but are at high risk of developing it. This preventive procedure is intended to significantly reduce the risk of breast cancer, especially in those with genetic predispositions or other high-risk factors.
This procedure is typically recommended for individuals at high risk of breast cancer, including:
Genetic Risk:
- BRCA1/BRCA2 Mutations: Women with these mutations have up to a 72% lifetime risk of breast cancer.
- Other gene mutations like PALB2, TP53, and CHEK2.
Strong Family History:
- Multiple close relatives (e.g., mother, sister, or daughter) diagnosed with breast or ovarian cancer, especially at a young age.
Personal Medical History:
- Previous cancer in one breast (may opt for removal of the other breast to prevent future cancer).
- History of atypical hyperplasia or lobular carcinoma in situ (LCIS), which are precancerous conditions.
Dense Breast Tissue:
- Dense tissue can make cancer harder to detect with imaging and may slightly increase cancer risk.
The decision to undergo a prophylactic mastectomy is highly personal and depends on:
- Your genetic risk profile.
- Family and personal medical history.
- Emotional readiness for the physical and psychological impact.
- Long-term lifestyle and health goals.
Consult with a genetic counselor, oncologist, and plastic surgeon to fully understand the risks, benefits, and alternatives before making a decision. Other options, such as enhanced screening or chemoprevention, may also be worth exploring for risk management.
FAQs
Does Breastfeeding Prevent Breast Cancer?
Breastfeeding has been shown to lower the risk of breast cancer, particularly for hormone-receptor-positive types. The protective effect occurs for several reasons. First, breastfeeding lowers estrogen levels in the body during lactation. Since some types of breast cancer are fueled by estrogen, this reduced exposure to the hormone can help decrease the risk.
Additionally, breastfeeding causes the body to shed breast tissue, potentially removing cells with DNA damage that could otherwise develop into cancer. Breastfeeding also delays the return of menstruation, which reduces lifetime exposure to estrogen and progesterone, further lowering cancer risk. Moreover, the act of breastfeeding induces changes in breast cells that may make them more resistant to cancerous transformations.
The protective effect of breastfeeding increases with the duration of breastfeeding. Research suggests that breastfeeding for at least 12 months (across all children) may reduce breast cancer risk by 4–5% per year of breastfeeding. The longer the duration, the greater the benefit. Exclusive breastfeeding, where no formula feeding is involved, seems to enhance this protective effect even further.
Does Breast Massage Prevent Cancer?
Breast massage does not prevent breast cancer. While some people believe that regular breast massage can help with early detection by making it easier to feel lumps or changes in the breast tissue, there is no scientific evidence to support the idea that breast massage itself can prevent the development of cancer.
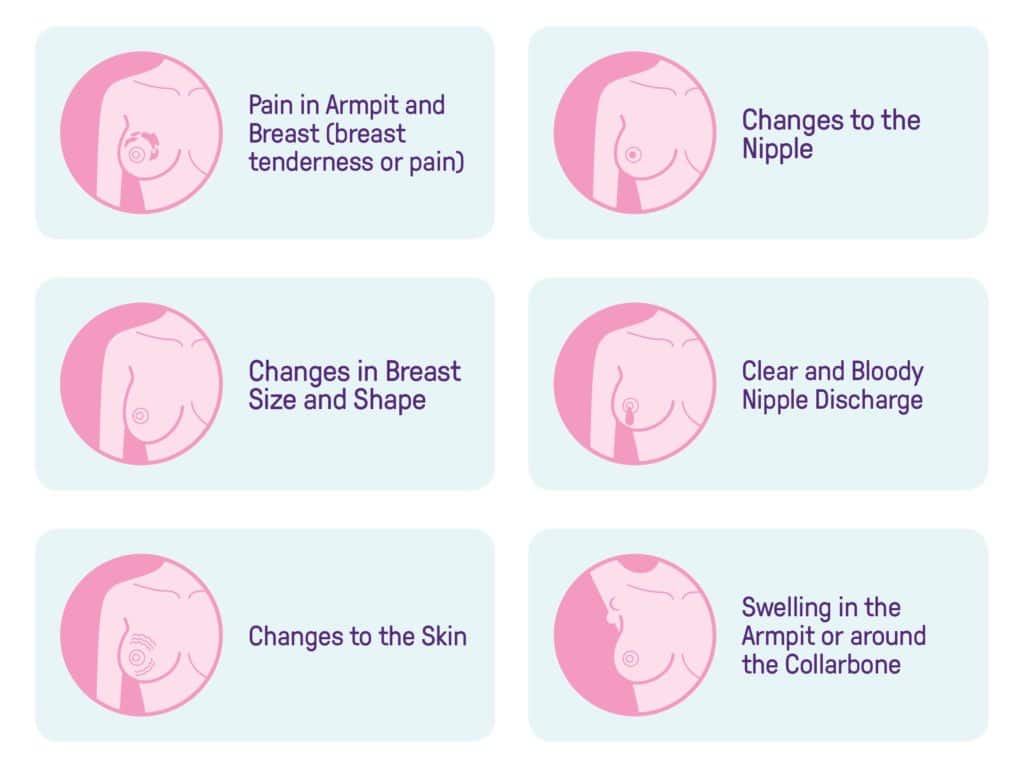
Breast cancer is a complex disease influenced by factors such as genetics, hormones, age, and lifestyle choices. While maintaining regular self-exams is an important part of breast health, it is the early detection of changes—such as lumps, thickening, or skin changes—that matters most for finding cancer at an early stage. However, breast massage is not a substitute for regular screenings, such as mammograms or clinical breast exams, which are proven to be more effective in detecting breast cancer.
Do Breast Implants Prevent Breast Cancer?
Breast implants do not prevent breast cancer. In fact, they do not offer any protective benefits against the development of breast cancer. While breast implants may change the appearance of the breasts, they do not affect the underlying risk factors associated with breast cancer, such as genetics, age, or lifestyle.
However, it is important to note that breast implants can make it more challenging to detect breast cancer through routine screening methods like mammograms. The implants can obscure breast tissue, potentially hiding tumors or making it more difficult for radiologists to interpret results accurately. Special imaging techniques, such as additional views during mammography or breast MRI, are sometimes used to help get clearer images for women with implants.
While breast implants themselves do not prevent cancer, they are not directly linked to an increased risk of breast cancer either. There are, however, certain rare conditions associated with breast implants, such as anaplastic large cell lymphoma (ALCL), a type of cancer that can develop in the tissue surrounding the implant. This is not the same as breast cancer but is an important consideration for women with implants.
Does Breast Reduction Prevent Breast Cancer?
Breast reduction surgery does not prevent breast cancer, but it may reduce some of the risks associated with the disease. The procedure involves the removal of excess breast tissue to reduce breast size and alleviate discomfort, particularly for women with very large breasts. While this can improve physical and emotional well-being, it does not eliminate the risk factors for breast cancer, such as genetics, age, or lifestyle.
One indirect benefit of breast reduction is that it can make it easier for individuals to perform regular self-breast exams and undergo screenings like mammograms. With smaller breasts, there may be less tissue to examine, which could lead to a more accurate detection of any potential changes or lumps. However, breast reduction does not remove all of the breast tissue, so regular screenings and exams are still necessary.
There is also some evidence that breast reduction might slightly lower the risk of developing breast cancer by removing some of the breast tissue that could potentially develop into cancer. However, this effect is minimal, and breast cancer prevention still largely depends on factors like genetics, lifestyle choices, and routine screening practices.
How You Can Help
We want to ensure no more lives are cut short by breast cancer. Support our life changing research with a donation, or participate in a clinical trial to help us to find a cure.